Association of Sociodemographic Factors and Blood Group Type With Risk of COVID-19 in a US Population
Jeffrey L. Anderson, MD; Heidi T. May, PhD, MSPH; Stacey Knight, PhD, MStat; Tami L. Bair, BS; Joseph B. Muhlestein, MD; Kirk U. Knowlton, MD; Benjamin D. Horne, PhD, MStat, MPH
Introduction
The observed variability in susceptibility to SARS-CoV-2 and severity of the ensuing COVID-19 have raised intense interest in their environmental and genetic risk factors. An early report from China1 suggested that blood group A was associated with increased susceptibility and blood group O was associated with reduced susceptibility to SARS-CoV-2 infection. These reports motivated widespread interest in examining ABO blood groups as potential COVID-19 risk factors. Subsequent studies from Italy and Spain2 reported that blood group A was associated with an increased risk of severe COVID-19 and blood group O was associated with a reduced risk. In contrast, a large Danish study3 implicated disease susceptibility but not severity. However, observations from Boston,45 Massachussets, and NewYork, NewYork, did not confirm any specific associations between ABO blood group and disease. The controversy raised by these contrasting reports led to this case-control study.
Methods
Our objective in this case-control study was to independently test whether blood type is associated with SARS-CoV-2 susceptibility and COVID-19 severity. The study was approved by the Intermountain Medical Center institutional review board with a waiver of consent because the study represented no more than minimal privacy risk to individuals. This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Intermountain Healthcare, a nonprofit, integrated health care system of 24 hospitals and 215 clinics in Utah, Idaho, and Nevada, generated a SARS-CoV-2 and COVID-19–specific electronic health records database. We searched this database for individuals who were tested for SARS-CoV-2 between March 3 and November 2, 2020, and had a recorded blood type. For individuals who underwent multiple tests, the first test with a positive result was chosen, otherwise the first test with a negative result was used. We compared positive vs negative test results, hospitalized vs nonhospitalized patients, and intensive care unit (ICU) vs non-ICU patients. Infectivity was determined by SARS-CoV-2–specific polymerase chain reaction testing of nasal swabs or saliva samples. Analysis of variance assessed associations across ABO groups. Odds ratios (ORs) between ABO groups were assessed by logistic regression adjusted for age, sex, and Rh factor. P values were 2-sided, and statistical significance was set at P < .167 for each of the 3 primary comparisons. Statistical significance was set at P = .006 for assessment of ORs because each set underwent 9 comparisons. Data were analyzed from November 20, 2020, to February 26, 2021.
Results
A total of 107 796 individuals (mean [SD] age, 42.0 [17.8] years; 82 875 [76.9%] women) who had been tested for SARS-CoV-2 infection were included in the study. Further demographic characteristics of the studied population and ABO blood group associations are shown in Table 1.
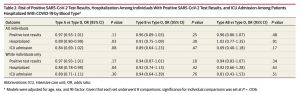
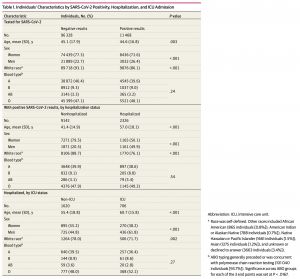 Among individuals with COVID-19, hospitalization was associated with male sex (1165 men [50.1%] hospitalized vs 1871 men [20.5%] not hospitalized) and age (mean [SD] age among hospitalized patients, 57.0 [18.1] years vs 41.4 [14.9] years among nonhospitalized individuals). Admission to an ICU was also associated with male sex (426 men [61.8%] admitted to ICUs vs 725 men [44.8%] not admitted) and age (mean [SD] age among patients admitted to ICUs, 60.7 [158] years vs 55.4 [18.8] years in patients not admitted). Non-White race, which included African American, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, Asian, and unknown or declined to answer, was associated with viral positivity (1592 individuals [13.9%] with positive results vs 6610 individuals [6.9%] with negative results) and hospitalization (556 patients [23.9%] hospitalized vs 1036 individuals [11.3%] not hospitalized). Blood type was not associated with disease susceptibility or severity, including viral positivity, hospitalization, or ICU admission (Table 1). Compared with type O blood, type A was not associated with increased viral positivity (OR, 0.97 [95% CI, 0.93-1.01]; P = .11), hospitalization (OR, 0.89 [95% CI, 0.80-0.99]; P = .03), or ICU admission (OR, 0.84 [95% CI, 0.69- 1.02]; P = .08) (Table 2). Similarly, types B and AB were not associated with worse outcomes than type O. Analyses restricted to White race produced similar results (Table 2).
Among individuals with COVID-19, hospitalization was associated with male sex (1165 men [50.1%] hospitalized vs 1871 men [20.5%] not hospitalized) and age (mean [SD] age among hospitalized patients, 57.0 [18.1] years vs 41.4 [14.9] years among nonhospitalized individuals). Admission to an ICU was also associated with male sex (426 men [61.8%] admitted to ICUs vs 725 men [44.8%] not admitted) and age (mean [SD] age among patients admitted to ICUs, 60.7 [158] years vs 55.4 [18.8] years in patients not admitted). Non-White race, which included African American, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, Asian, and unknown or declined to answer, was associated with viral positivity (1592 individuals [13.9%] with positive results vs 6610 individuals [6.9%] with negative results) and hospitalization (556 patients [23.9%] hospitalized vs 1036 individuals [11.3%] not hospitalized). Blood type was not associated with disease susceptibility or severity, including viral positivity, hospitalization, or ICU admission (Table 1). Compared with type O blood, type A was not associated with increased viral positivity (OR, 0.97 [95% CI, 0.93-1.01]; P = .11), hospitalization (OR, 0.89 [95% CI, 0.80-0.99]; P = .03), or ICU admission (OR, 0.84 [95% CI, 0.69- 1.02]; P = .08) (Table 2). Similarly, types B and AB were not associated with worse outcomes than type O. Analyses restricted to White race produced similar results (Table 2).
With contrasting reports from China(1), Europe(2,3), Boston(4), New York(5), and elsewhere(6), we embarked on a large, prospective case-control study that included more than 11,000 individuals who were newly infected with SARS-CoV-2, and we found no ABO associations with either disease susceptibility or severity. The smaller sample sizes and retrospective, observational nature of many prior studies, in addition to their striking heterogeneity of ABO associations with disease susceptibility and severity, could be due to chance variations, publication bias, differences in genetic background, geography and environment, and viral strains. The ABO gene is highly polymorphic, and ABO blood groups are distributed differently across ancestries and geographies. Differing disease susceptibilities could be due to natural antibodies or prothrombotic effects with non group O(6). The Utah population is dominated by Northern European ancestry, with a minority contribution of Hispanic/Latinx and other ethnicities. However, our results are similar among individuals of White race alone.
Given the large and prospective nature of our study and its strongly null results, we believe that important associations of SARS-CoV-2 and COVID-19 with ABO groups are unlikely and will not be useful factors associated with disease susceptibility or severity on either an individual or population level for similar environments and ancestries. Additional studies, closely controlled for genetics, geography, and viral strain, are required before accepting blood group as a determinant of predisposition to or severity of COVID-19.
ARTICLE INFORMATION
Accepted for Publication: March 3, 2021.
Published: April 5, 2021. doi:10.1001/jamanetworkopen.2021.7429
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2021 Anderson JL et al. JAMA Network Open.
Corresponding Author: Jeffrey L. Anderson, MD, Intermountain Medical Center Heart Institute, 5121 S Cottonwood St, Bldg 4, 6th Floor, Murray, UT 84107 (jeffreyl.anderson@imail.org).
Author Affiliations: Intermountain Medical Center Heart Institute, Salt Lake City, Utah (Anderson, May, Knight, Bair, Muhlestein, Knowlton, Horne); University of Utah School of Medicine, Salt Lake City (Anderson, Knight, Muhlestein, Knowlton); Stanford University, Stanford, California (Horne).
Author Contributions: Dr May and Ms Bair had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Anderson, Muhlestein, Knowlton.
Acquisition, analysis, or interpretation of data: Anderson, May, Knight, Bair, Muhlestein, Horne.
Drafting of the manuscript: Anderson, May, Knight.
Critical revision of the manuscript for important intellectual content: Anderson, Bair, Muhlestein, Knowlton, Horne. Statistical analysis: May, Knight.
Obtained funding: Anderson.
Administrative, technical, or material support: Anderson, Bair, Muhlestein, Knowlton, Horne.
Supervision: Anderson, Muhlestein, Knowlton, Horne.
Conflict of Interest Disclosures: Dr Muhlestein reported receiving a research endowment from Dell Loy Hansen Heart Foundation Heart Institute during the conduct of the study. Dr Horne reported receiving grants from Intermountain Research and Medical Foundation, AstraZeneca, and PCORnet; nonfinancial support in the form of in-kind donations from GlaxoSmithKline and CareCentra; serving on an advisory board for LabMe.ai; and licensing of intellectual property from Alluceo and CareCentra outside the submitted work. No other disclosures were reported.
Additional Contributions: Brianna Ronnow, MS (Intermountain Healthcare), assisted with manuscript submission and was not compensated for the work.
REFERENCES
1. LiJ,WangX,ChenJ,CaiY,DengA,YangM.AssociationbetweenABObloodgroupsandriskofSARS-CoV-2 pneumonia. Br J Haematol. 2020;190(1):24-27. doi:10.1111/bjh.16797
2. EllinghausD,DegenhardtF,BujandaL,etal;SevereCovid-19GWASGroup.Genomewideassociationstudyof severe Covid-19 with respiratory failure. N Engl J Med. 2020;383(16):1522-1534. doi:10.1056/NEJMoa2020283
3. BarnkobMB,PottegårdA,StøvringH,etal.ReducedprevalenceofSARS-CoV-2infectioninABObloodgroup O. Blood Adv. 2020;4(20):4990-4993. doi:10.1182/bloodadvances.2020002657
4. LatzCA,DeCarloC,BoitanoL,etal.BloodtypeandoutcomesinpatientswithCOVID-19.AnnHematol.2020; 99(9):2113-2118. doi:10.1007/s00277-020-04169-1
5. ZietzM,ZuckerJ,TatonettiNP.AssociationsbetweenbloodtypeandCOVID-19infection,intubation,and death. Nat Commun. 2020;11(1):5761. doi:10.1038/s41467-020-19623-x
6. PenduJL,BreimanA,RocherJ,DionM,Ruvoën-ClouetN.ABObloodtypesandCOVID-19:spurious,anecdotal, or truly important relationships: a reasoned review of available data. Viruses. 2021;13(2):160. doi:10.3390/ v13020160
JAMA Network Open. 2021;4(4):e217429. doi:10.1001/jamanetworkopen.2021.7429