Obesity Is Deadlier in Men With COVID-19 Than in Women
Becky McCall
May 6, 2021 (Medscape) – The association between obesity and poor outcomes in COVID-19 are worse in men than women, with increased rates of in-hospital death, shows the largest study to date exploring the different impact of obesity between the sexes on COVID- 19.
Men with a body mass index (BMI) greater than 35 kg/m , and women with a BMI of 40 kg/m or more, were significantly more likely to die in hospital with COVID-19 than patients with a “normal” BMI of 18.5-24.9 kg/m .
“Particular attention should be paid in protecting the population living with severe obesity from SARS-CoV-2 with priority to vaccination access, remote work, telemedicine, and other measures,” write Arcelia Guerson-Gil, MD, of the University Hospital for Albert Einstein College of Medicine, New York City, and colleagues.
And “patients with severe obesity diagnosed with COVID-19 should be treated with particular attention given the high risk for worse outcomes,” they stress.
The study was published May 6 in the European Journal of Clinical Microbiology & Infectious Diseases.
Classes of Obesity Most Likely to Lead to Poor COVID-19 Outcomes
Other studies have shown an association between worse overall COVID-19 outcomes and older age, male sex, and a number of comorbidities including obesity, which has been shown to be an independent risk factor for hospitalization, severe disease, and mortality in patients with COVID-19.
But the question remains as to whether all classes of obesity are prone to worse outcomes in COVID-19 or whether this is specific to severe obesity alone.
As a primary outcome, researchers looked at which classes of obesity are associated with higher in-hospital mortality and whether this is sex-linked.
The association between obesity and systemic inflammation (via IL-6 levels) was also assessed, given that a major cause of COVID-19 severity and death is an excessive inflammatory response.
The large, single-center, retrospective study of patients admitted to hospital between March and May 2020 (some in intensive care) with COVID-19 included 3530 patients, 1579 of whom were women and all of whom were aged 18 years or older.
Patients were classified into six groups according to BMI: 896 had a BMI < 25 kg/m , 1162 had a BMI of 25-29 kg/m , 809 had a BMI of 30-34 kg/m2 (class I obesity), and 663 had a BMI of 35 kg/m2 or higher (class II and III obesity).
Associations were explored between these groups and in-hospital mortality, need for intubation, and development of severe pneumonia.
Men With Severe Obesity Drove Association With In-Hospital Death
The odds ratios (ORs) for in-hospital death were higher for men of a given BMI than women (compared with the reference group of a BMI of 18.5-24.9 kg/m2), even after adjusting for other potential confounders, such as age, hypertension, diabetes, coronary artery disease, and chronic kidney disease (Table). Table. Sex-Based Subgroup Analysis for the Outcome of Mortality
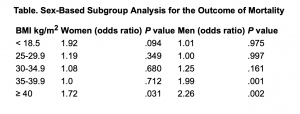 Obesity classes II and III in men and obesity class III in women were independently associated with higher in-hospital mortality in patients with COVID-19, and the male population with severe obesity mainly drove the association.
Obesity classes II and III in men and obesity class III in women were independently associated with higher in-hospital mortality in patients with COVID-19, and the male population with severe obesity mainly drove the association.
For severe pneumonia, those with a BMI ≥ 40 kg/m2 had an OR of 1.61 (P = .001) compared with normal BMI, those with a BMI ≥ 35 kg/m2 had an OR of 1.71 (P < .001), and those with a BMI ≥ 30 kg/m2 had an OR of 1.57 (P < .001).
For intubation, those patients with a BMI ≥ 40 kg/m2 had an OR of 1.58 (P = .005), those with a BMI ≥ 35 kg/m2 had an OR of 1.68 (P < .001), and those with a BMI ≥ 30 kg/m2 had an OR of 1.77 (P < .001).
Also, underweight patients — those with a BMI < 18.5 kg/m2 — were found to have an increased predicted probability of mortality.
Is it Down to Differing Body Shapes Between Women and Men?
The researchers note fat tissue distribution differs in men and women, which “might help explain the disproportionate impact of severe obesity in the outcomes of men compared to women.”
“Men tend to have more adipose tissue distributed in the central or abdominal region, also known as the android phenotype, whereas women tend to have more peripherally distributed subcutaneous fat, also known as the gynoid phenotype. The android phenotype carries greatest risk for metabolic disorders. The gynoid phenotype may have a less inflammatory phenotype,” write the authors.
“In contrast, visceral fat has been shown to demonstrate greater proinflammatory characteristics than subcutaneous fat. In addition, excessive visceral adipose tissue has a negative impact on lung function by reducing chest wall compliance, forced expiratory volume, and forced vital capacity,” they explain.
No Interplay Between IL-6 and BMI in Study
The researchers suspected there may be an association between BMI and systemic inflammation as indicated by IL-6 levels. “However, we found that this wasn’t the case,” noted Guerson-Gil in a press statement.
“Either predisposition to systemic hyper-inflammation may be a less important pathophysiologic mechanism behind worse outcomes in patients with severe obesity or this effect is not strongly mediated by IL-6 and other factors may play a role,” she and her coauthors say.
They also caution that the retrospective study design does not allow for conclusions about cause and effect, and that the rapidly changing management of patients with COVID-19 during the first wave of the pandemic might have affected the results.
Further studies are needed to confirm the findings and pilot clinical trials would be useful to assess whether drugs targeting visceral adipose tissue may improve outcomes.
The authors have reported no conflicts of interest.
Eur J Clin Microbiol Infect Dis. Published May 6, 2021.

